What Does Low AMH or Low Ovarian Reserve Mean?
Medically Reviewed By Dr. Pamela Frank, BSc, Naturopathic Doctor
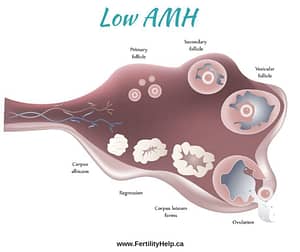
The term ovarian reserve refers to a woman’s remaining capacity to continue to produce eggs. This term is also sometimes used to estimate her remaining number of egg follicles and chances of success with fertility treatment.
What is AMH or Anti-Mullerian Hormone?
AMH is a hormone that is released as egg follicles are developing into an egg. It is only released when egg follicles are in the mid-stages of developing, that is, when they are less than 9 mm in diameter. An egg follicle is normally 18-24 mm when it releases the egg at ovulation. Dormant egg follicles, or primordial follicles, are the ones that have been in the ovaries since you were born. These follicles are just resting, waiting for their turn to become eggs and therefore they do not secrete AMH.
What does an AMH test actually mean?
Since AMH is only secreted by follicles that have started to develop but that are less than 9 mm in size, the information provided by this test is limited. Therefore, AMH is only a reflection of how many follicles are in the early stages of development. A normal AMH can indicate that there are a normal number of follicles in development between resting and 9 mm. A high AMH can indicate more than average egg follicles in this stage. Women with PCOS have a high AMH because their follicles are stuck in the early stages of development due to the hormonal imbalances that accompany PCOS.
A low AMH was thought to indicate a low number of remaining egg follicles (resting/primordial follicles or ovarian reserve) and therefore, decreased odds of conception. Recent research has disproved this assumption. Therefore, all that a low AMH means is that not many follicles are in the early stages of development. However, there are many factors that influence how many follicles are developing at a given time. Negatively interpreting a low AMH, particularly in a younger woman, creates a false and unnecessary sense of despair. Many of the women that I have helped conceive and have healthy babies were told that they had a low AMH, low ovarian reserve, a poor chance of conceiving on their own, would need egg donors, etc. These dire predictions based solely on a low AMH are completely unwarranted. In some women, particularly those approaching menopause, a low AMH can be indicative of the above, but each individual’s AMH needs to be interpreted in the context of all of the factors affecting her fertility.
What is a Normal AMH Level?
Very high AMH is anything greater than 28.5 pmol/L. This is thought to be a sign of PCOS or polycystic ovarian syndrome where many egg follicles are stuck in the early stages of development. It is correctable by addressing and normalizing the hormone imbalances associated with PCOS. There is more information on that here.
Normal AMH = 10.7 – 28.5 pmol/L
Low normal AMH = 7.1 – 10.7 pmol/L
Low AMH = 3.6 – 7.1 pmol/L
Very low AMH = less than 3.6 pmol/L
What is the Cause of a Low AMH?
There are several possible causes of a low AMH. Low AMH is only an indicator that not many follicles are in the midst of developing into larger ones. There are several reasons why this can happen. Generally speaking, anything that is suppressing egg development will cause a low AMH.
What Might Suppress Egg Follicle Development and Contribute to a Low AMH/Ovarian Reserve Test?
Certain hormones suppress the function of the ovaries:
- Testosterone – High testosterone, high-normal testosterone or even slightly high levels can slow egg development, leaving many follicles stuck at less than 9 mm and therefore AMH levels are very high, as in PCOS.
- Prolactin – Prolactin is the hormone that is made to help with breastfeeding. While a woman is nursing a newborn, prolactin levels are high, which can suppress ovulation (although this is not a reliable means of birth control). Prolactin may also be high in women who are under high levels of stress. In that situation, it can also suppress egg follicle development and cause AMH to be low.
- Underactive thyroid – Your thyroid is like the gas pedal for your body. When the thyroid is underworking or you are hypothyroid, there isn’t enough gas going to the ovaries to allow the ovaries to work normally. In this case, the ovaries may not be developing enough egg follicles and AMH may be low. Correcting your thyroid dysfunction is the key to resolving AMH in this case.
- Low estradiol. For egg follicles to develop, they have to release estrogen or estradiol. In order to build estrogen, your ovaries need a steady supply of testosterone. About half of your testosterone is produced by your adrenal or stress glands. If your adrenals or HPA axis are not working well, they may not be supporting the ovaries to produce sufficient estradiol to allow follicles to mature. Supporting the endocrine system (pituitary, adrenal glands, thyroid and ovaries), normalizes AMH in this case.
- Low Vitamin D – Vitamin D reduces inflammation and may improve egg follicle development in women with PCOS. Vitamin D supplementation has also been shown to improve AMH levels.
- Autoimmune disorders – Research on autoimmune disorders, like lupus, has shown significantly higher estradiol levels and lower AMH levels than in control groups. Autoimmune conditions can be successfully treated through naturopathic medicine.
What Does Having a Low AMH Mean for Fertility?
As a naturopathic doctor, low AMH signifies a need to correct the underlying problem that is causing it. It does not indicate that a woman must undergo expensive, invasive fertility treatments, at least not for all women with low AMH. A recent study concluded that “among women attempting to conceive naturally, a diminished ovarian reserve was not associated with infertility; women should be cautioned against using AMH levels to assess their current fertility.”
Low AMH Research
Vitamin D
Irani M, Merhi Z. Role of vitamin D in ovarian physiology and its implication in reproduction: a systematic review. Fertil Steril. 2014 Aug;102(2):460-468.e3. doi: 10.1016/j.fertnstert.2014.04.046. Epub 2014 Jun 3. https://www.ncbi.nlm.nih.gov/pubmed/24933120
Testosterone
P. Pinola, L.C. Morin-Papunen, A. Bloigu, K. Puukka, A. Ruokonen, M.-R. Järvelin, S. Franks, J.S. Tapanainen, and H. Lashen Anti-Müllerian hormone: correlation with testosterone and oligo- or amenorrhoea in female adolescence in a population-based cohort study. Hum Reprod. 2014 Oct 10; 29(10): 2317–2325.
Published online 2014 Jul 23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4164146/
Lupus
Wenhong Ma, PhD, Zhongping Zhan, MM, Xiaoyan Liang, MD, Jianhui Chen, BM, Xingfang Huang, MM, and Caiyun Liao, MD. Subclinical Impairment of Ovarian Reserve in Systemic Lupus Erythematosus Patients with Normal Menstruation Not Using Alkylating Therapy. J Women’s Health (Larchmt). 2013 Dec; 22(12): 1023–1027.
Low AMH
Anne Z. Steiner, MD, MPH; David Pritchard, MS; Frank Z. Stanczyk, PhD; et al James S. Kesner, PhD; Juliana W. Meadows, PhD; Amy H. Herring, ScD; Donna D. Baird, PhD, MPH. Association Between Biomarkers of Ovarian Reserve and Infertility Among Older Women of Reproductive Age. JAMA. 2017;318(14):1367-1376.